Spread the Word! Celebrating Hip-Hop Fusion: Future, Metro Boomin, & J. Cole Collab! 🎵 | Jcole | WeStillDontTrustYou | HipHopCollab | MusicIndustry ...


Spread the Word! Celebrating Hip-Hop Fusion: Future, Metro Boomin, & J. Cole Collab! 🎵 | Jcole | WeStillDontTrustYou | HipHopCollab | MusicIndustry ...

Explore how the NBA's New Orleans Pelicans, led by Zion Williamson, are transforming into a formidable basketball force. ...

Spread the Word! Dive into the World of Rolex Deepsea Full Gold & Blue Edition ⌚✨ | Rolex | LuxuryWatches | ...
Spread the Word! Championship Dreams: Russell Westbrook’s Game-Changing Role with the Clippers 🏀 Can He Lead Them to Victory? | NBA ...

Spread the Word! Deciphering the Morgan Wallen Incident: Exploring Reckless Endangerment Charges 🎵 | MorganWallen | RecklessEndangerment | CelebrityScandal | LegalNews ...

Spread the Word! Remembering Chance Perdomo: A Tribute to a Talented Star | ChancePerdomo | InMemoriam | ChillingAdventures | GenV | ...
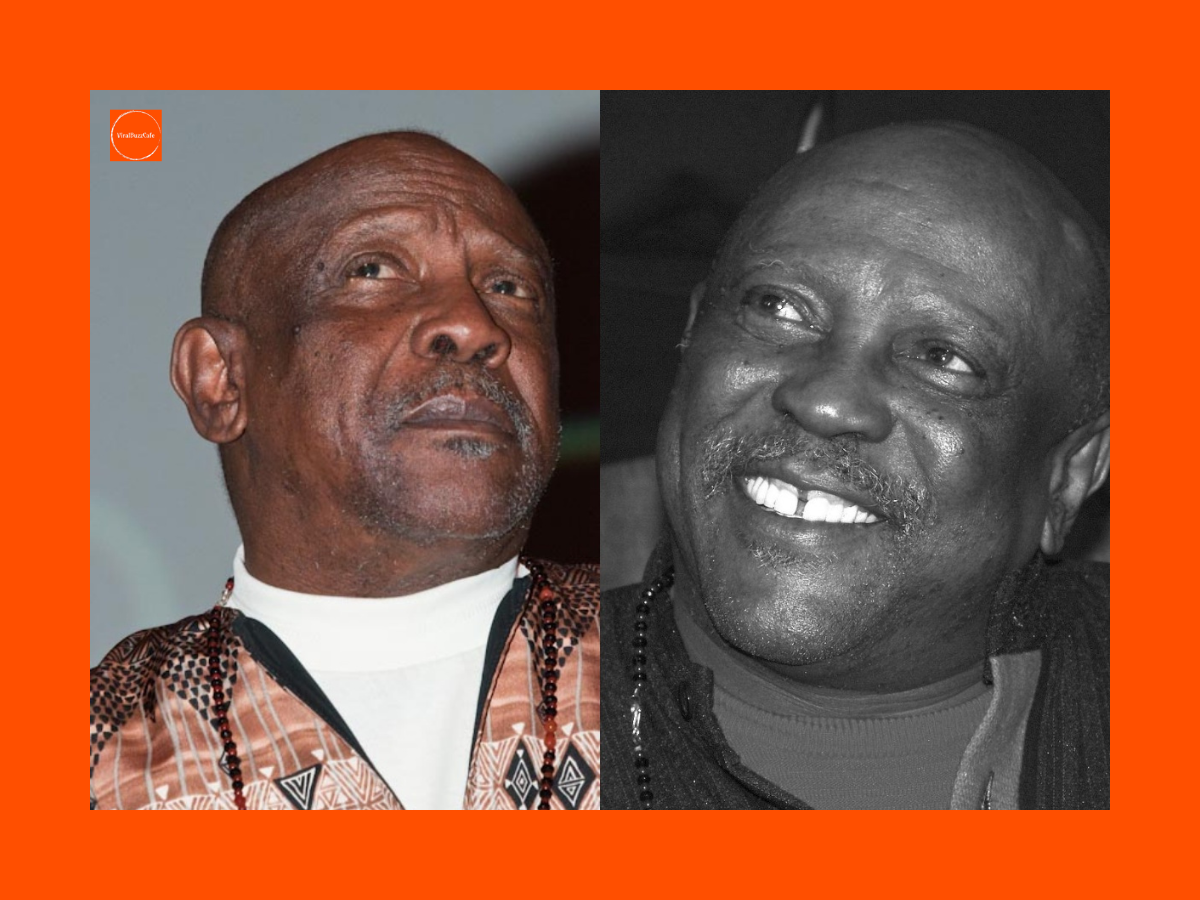
Spread the Word! Louis Gossett Jr., 87, Dies: Remembering the Legacy of an Iconic Actor 🎥🌟 | LouisGossettJr | HollywoodIcon | ...

Spread the Word! 🥃 Raise a Glass: Celebrating World Whisky Day: March 27th Around the Globe 🌍 | WhiskyLovers | WorldWhiskyDay | ...

Spread the Word! Volvo EX90 Launches in USA with Top Safety & Performance Features! | VolvoEX90 | SUV | SafetyFirst | ...
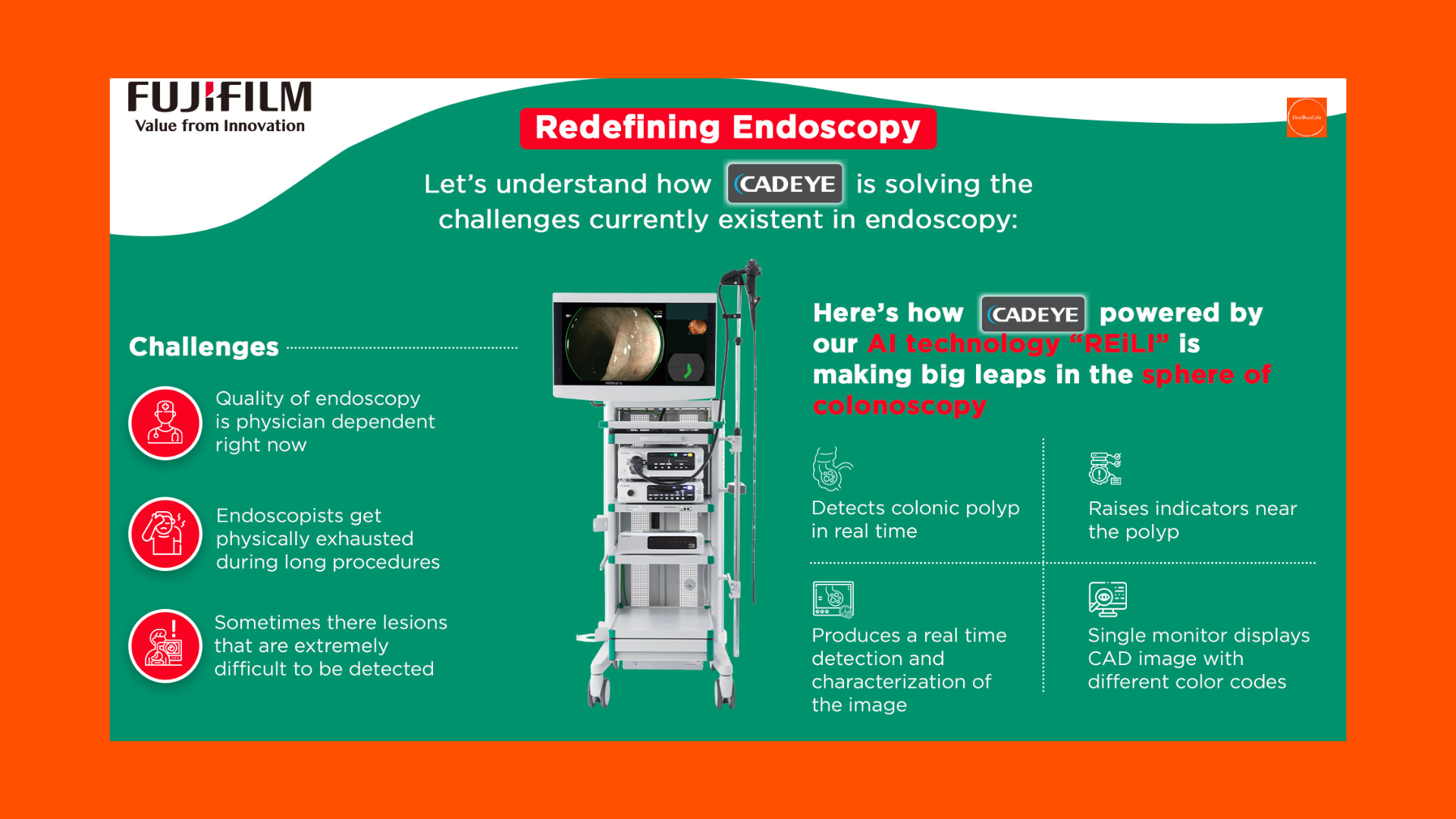
Spread the Word! Future of Colonic Health: CAD EYE® Revolutionizes Polyp Detection! | CADeye | ColonicHealth | MedicalInnovation | HealthTech | ...